Symptoms, Diagnosis & Testing
Recognize Gaucher disease type 1 and understand the
consequences of
delayed diagnosis and treatment.
Recognizing symptoms of Gaucher disease type 1
Gaucher disease is an inherited, autosomal recessive lifelong condition marked by extreme diversity in genotype, phenotype, age of onset, and disease severity, as well as an unpredictable, progressive disease course.1,6 Signs, symptoms, and clinical course may differ even among individuals with the same genotype and within the same family.7 It may also display inactive periods interrupted by episodes of acute crisis or evidence of disease advancement. Patients may appear to be asymptomatic, yet harbor disease manifestations such as cytopenia, splenomegaly, or osteopenia.1,2 Symptoms should not be ignored, as this progressive condition may lead to further medical complications.1
Symptoms are
diverse,
unpredictable, and variable1,6,7
Onset may occur at any age
Some patients may be asymptomatic
while others may experience one or
more symptoms
The nature and severity of some
symptoms may fluctuate as
disease
progresses
Signs and symptoms
The signs and symptoms of Gaucher disease type 1 may not be obvious. The early signs and symptoms of Gaucher disease type 1 tend to reflect the hematologic aspects of the disease, but skeletal manifestations are often present.2
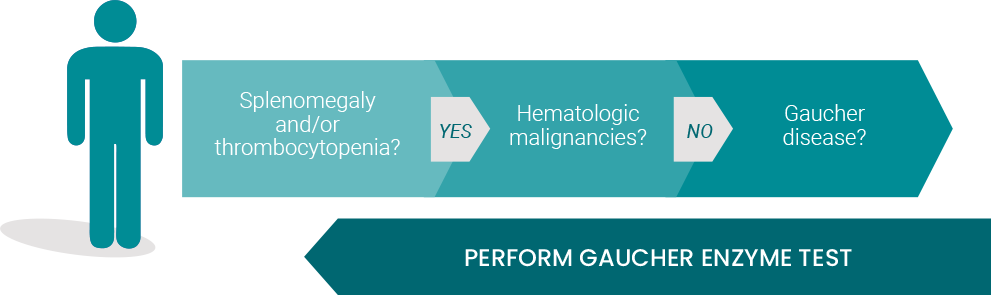
- Splenomegaly and/or thrombocytopenia are 2 of the most prominent and frequent symptoms6
- Hepatomegaly, anemia, and bone disease are also common3,6
- Symptoms often mimic the signs of hematologic malignancies (ie, leukemia, lymphoma, or multiple myeloma)1
- Symptoms can begin at any age, and the clinical progression ranges from asymptomatic to life-threatening1,6
- Growth failure can occur in children8
INCIDENCE OF MANIFESTATIONS IN UNTREATED GAUCHER DISEASE TYPE 18-10
Anemia 40%
Moderate to Severe Hepatomegaly 87%
Moderate to Severe Thrombocytopenia 50%
Moderate to Severe Splenomegaly 95%
Bone Disease:
- Radiologic Evidence 81%
- Bone Pain 27%
- Bone Crisis 9%
Delayed Growth 34%
Cytopenias:
- Anemia 64%
- Thrombocytopenia 56%
Hepatomegaly 79%
Lung manifestations 1% to 2%
Splenomegaly 87%
Bone Pathologies:
- Bone pain 63%
- Erlenmeyer Flask Deformity 46%
- Osteopenia 42%
- Bone Crisis 33%
- Avascular Necrosis 25%
- Pathologic Fracture 15%
- Joint Replacement 8%
Splenomegaly and/or thrombocytopenia are among
the
2 most prominent and frequent presenting
symptoms
of Gaucher disease type 12,3
A delayed diagnosis can lead to further disease progression and multisystemic complications.1
Consequences of delayed diagnosis
When the diagnosis is missed, a patient with Gaucher disease type 1 may experience delays for up to 10 years. Gaucher disease type 1 is progressive and over time may lead to1,2,11:
- Bleeding due to thrombocytopenia/
coagulopathy, anemia - Progressive visceral enlargement
- Bone pain, osteonecrosis and fractures
- Growth failure in children
- Cytokine storm
- Markedly reduced quality of life
- Shortened life and increased cancer risk
Early diagnosis and proper management remain important, as damage caused by Gaucher disease type 1 may be irreversible1,2
It takes only 1 simple blood test to make a diagnosis if you suspect Gaucher disease. Visit GaucherCare.com to learn more about the Gaucher enzyme test.
Suspect Gaucher disease? Test to know
- β-Glucosidase enzyme assay is the standard, recommended method for establishing a confirmatory diagnosis of Gaucher disease, which is demonstrated by deficiency of β-glucosidase activity2
- Molecular testing (DNA) can be used to confirm the type of Gaucher disease as well as carrier status2,6
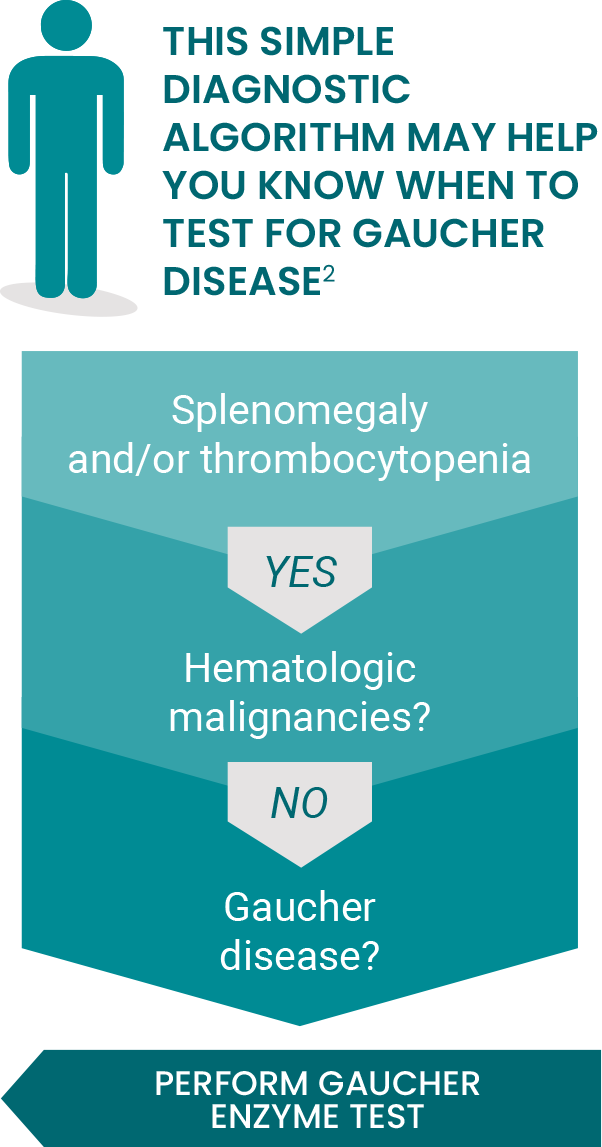
Don’t miss a Gaucher disease diagnosis. Test to know. It’s just a simple blood-based enzyme assay (ß-glucosidase).2*
*The above algorithm is for the general population. Gaucher disease type 1 is more prevalent in individuals of Ashkenazi Jewish descent and should be investigated before hematologic malignancies.
When an ERT is needed, choose the longest-approved therapy
Learn more